Do you have varicose veins? You’re not alone: 30% of adults in developed countries live with this condition(1).
For some, varicose veins are a cosmetic problem. For others, they might be a sign of a more serious disease.
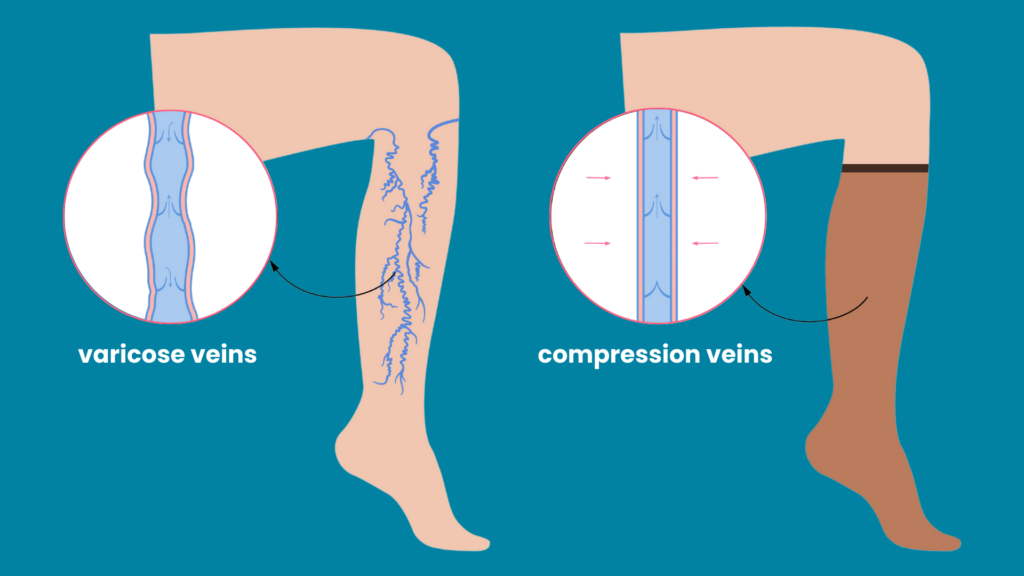
Normally, veins are not very visible. But when we develop varicose veins, they begin to bulge. The veins in your lower legs might appear blue or purple.
Varicose veins can be an early sign of venous insufficiency. Genetics can also play a large role in the development of varicose veins. Those in the latter group can have weaker vein walls, leading to varicose veins.
But what is the best way to treat varicose veins?
Compression therapy is the most recommended treatment(2). Read on to learn the basics of varicose veins and all you need to know about compression stockings.

Table of Contents
ToggleSigns and Symptoms of Varicose Veins
The first step toward treatment is determining if you have varicose veins in the first place.
Patients with varicose veins might have the following symptoms:
- Bluish purple veins in your lower limbs
- Bumpy and bulging vein texture
- “Spider veins”
- Skin changes near your veins, such as a “leathery” texture of discoloration
- Swelling of the lower limbs
- Venous ulcers, or open lesions
You might not experience obvious symptoms at first. Pay close attention if you start to feel:
- Itchy lower limbs
- Heaviness in your legs
- Throbbing and burning of the swollen legs
- Pain in the lower limbs after prolonged sitting and standing
- Bleeding from the varicose veins
If you think you have varicose veins, make an appointment with your doctor. They can review your symptoms and determine the best treatment option.
Treatment of Varicose Veins
Varicose vein treatment is usually sought out for cosmetic reasons. Your doctor will most likely recommend compression therapy to treat your symptoms.
Depending on your disease, your doctor might recommend other treatments like geothermal ablation, radiofrequency ablation, sclerotherapy, or surgical procedures.
Compression therapy is the easiest and most accessible, so it’s best to start there.
What is Compression Therapy?
Compression therapy is the gold standard of varicose veins treatment. It is a non-invasive treatment ideal for those looking to avoid surgical interventions. Options include elastic and non-elastic bandages, boots, hosiery, or stockings(5).
Compression therapy is also recommended for other ailments like lymphatic insufficiency, deep vein thrombosis, and post-thrombotic syndrome(5).
How Do Compression Stockings Work?
Compression stockings exert pressure on the lower legs. They are typically tightest at the ankles and loosen up the leg(5). This gradient pressure keeps blood from flowing downward.
Unlike arteries, veins are compressible. Compression decreases vein diameter, increasing the speed and volume of blood flow(6). The stockings can also reduce inflammation(5), pain, heaviness, and swelling (7).
Types of Compression Stockings
Graduated or medical compression stockings
Graduated compression stockings squeeze the legs. They are available at pharmacies in different styles and pressure amounts.
Stockings can be knee- or thigh-high and made of different materials. They are elastic or inelastic.
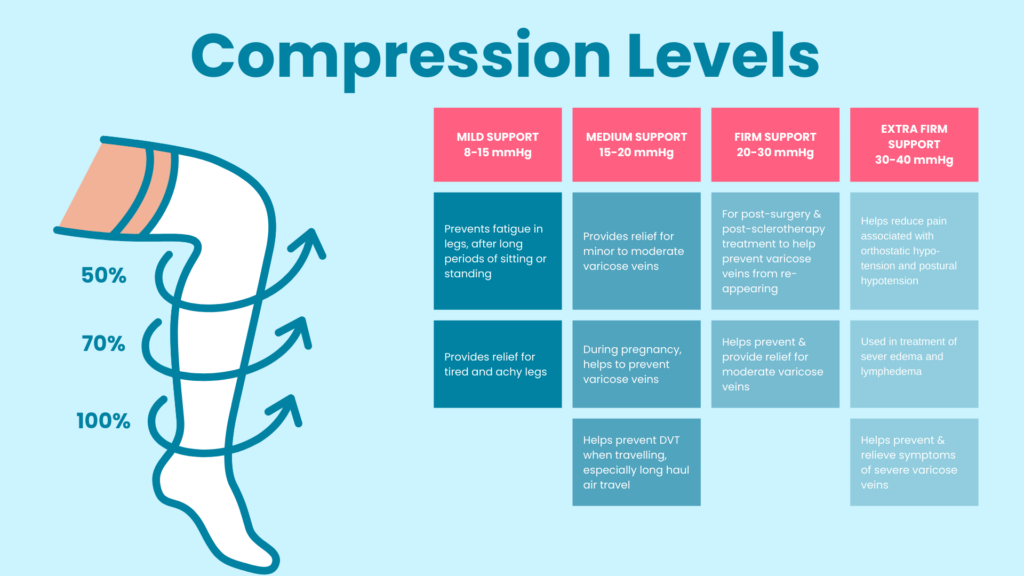
While there are no formal pressure standards, they are generally grouped into 4 levels(8):
Mild compression stockings are the lightest compression option, exerting 8-15mmHG of pressure. They relieve painful and crampy legs and are great for those who sit or stand for long periods. These are available over the counter–no prescription is required.
Class 1, or moderate compression stockings, are the lightest medical-grade compression stockings. They exert 15-20mmHg of pressure. Doctors prescribe these for mild vein disease to improve circulation. Class 1 stockings also help prevent deep vein thrombosis. They are sometimes recommended for athletes and to help manage swelling from pregnancy.
Class 2 stockings are strong compression stockings. These stockings provide 20-30mmHG of pressure. Doctors prescribe them for moderate edema, varicose veins, and deep vein thrombosis. They can help venous ulcers heal and are recommended post-surgery and post-sclerotherapy.
Class 3 compression stockings are the highest level of compression available at 30-40mmHg. These compression stockings are only available by prescription for serious vein conditions. These can also help prevent deep vein thrombosis.
Elasticity, leg size and shape, and patient activity all impact stocking pressure(5).
Doctors recommend graduated compression stockings to manage varicose veins and chronic venous insufficiency. They can also help patients manage venous ulcers and manifestations of post-thrombotic syndrome.
Anti-embolism stockings
Like graduated compression stockings, anti-embolism stockings provide graduated compression(5). These help prevent deep vein thrombosis by increasing blood flow and promoting venous return(9).
Knee-high and thigh-high versions are available. Unlike medical compression stockings, anti-embolism stockings are for bedridden patients.
Non-medical support hosiery
Non-medical support hosiery includes flight socks and elastic support stockings(5). They are ideal for those standing for long periods. Teachers, flight attendants, and nurses may wear these stockings.
The pressure is uniform and lower than that of graduated compression stockings. You can buy these in stores.
When Do You Need Compression Therapy?
Compression stockings help with several conditions:
Varicose Veins
Compression stockings are the standard treatment for varicose veins symptoms. They improve circulation to reduce blood stasis. They may be a standalone treatment or used in conjunction with sclerotherapy. Compression stockings can reduce blood clots and prevent skin discoloration by minimizing inflammation(5).
Chronic Venous Insufficiency
Compression stockings are also recommended for those with venous insufficiency. They can improve skin conditions such as eczema, induration, and lipodermatosclerosis(10). At higher pressure levels, they can help reduce the recurrence of venous ulcers.
Acute Stage of Deep Vein Thrombosis
Patients who wear compression stockings reduce their chances of developing DVT. Compression therapy is also effective alongside effective anticoagulant therapy(5).
Compression stockings are also recommended for lymphedema and edema. They’re recommended for pregnancy symptom management as well.
Contraindications of Compression Therapy
Compression stockings are not recommended for all patients. Tell your doctor if you have a history of the following:
- Severe congestive heart failure
- Severe leg edema
- Critical limb ischemia
- Peripheral neuropathy or other sensory impairment
- Extreme deformity of the leg, or unusual leg shape
- Fragile skin over bony areas
- Dermatitis
- Allergy to certain fabrics
Complications of Compression Stockings
Compression stocking complications can be avoided(5). Proper assessment, measurement, and fitting help prevent allergic reactions and skin issues.
If you experience any issues, talk to your doctor about trying different materials or pressure levels.
How to Effectively Use Compression Stockings
Some patients have trouble wearing compression stockings. They may experience sweating or itching. They may dislike the cost or cosmetic appearance of the stockings. They may even experience edema exacerbation or lesion exudation(11). Some may struggle to put the stockings on.
But compression stockings are only effective if you wear them! Note the fitting, material, and compression level to ensure a good fit. Then you’ll be more likely to wear them.
To ensure the best fit, measure your ankle at the narrowest part of your ankle bone. Measure your calf at the widest part while sitting down, with your leg at a 50-degree angle from your knee joint.
Wearing and Maintaining Your Compression Stockings
Before putting stockings on:
- Hand wash your compression stockings so they are more flexible and easier to put on.
- The best time to put on your stockings is after you bathe.
- If you have an open wound, make sure to dress it beforehand.
- Make sure that your legs are dry before putting stockings on.
When it’s time to put on your stockings:
- Sit in a chair with a back.
- Grasp the top of the stocking with one hand and reach inside towards the toe part with your other hand.
- Roll the stocking inside out to avoid stretching.
- Slowly roll and slide the stocking onto your heel and pull upwards gradually.
- Take your time when putting your stockings on. This will make the process easier!
Conclusion
Compression stockings are still the first-line treatment for varicose veins. They increase blood flow, decrease blood volume, and reduce reflux and venous hypertension.
This treatment can reduce inflammation and edema. Talk to your doctor to weigh the benefits and risks of using compression stockings.
Measurements and pressure amounts depend on the severity of your varicose veins. The worse your symptoms and disease, the stronger the degree of compression. It’s also important to wear your stockings to get the benefits of treatment.
Ready to seek treatment for your varicose veins? Connect with Elite Vein Clinic. Our experts will evaluate your condition and medical history. From there, they will provide proper compression therapy guidance. Find Elite Vein Clinic in Phoenix, Chandler, Gilbert, Mesa, Scottsdale, Tempe, and Peoria. Don’t wait one day longer to improve your vein health: book your free consultation today!
References
- Shadrina, A.S., Sharapov, S.Z., Shashkova, T.I., & Tsepilove, Y.A. (2019). Varicose veins of lower extremities: Insights from the first large-scale genetic study. PLOS Genetics 15(4). https://doi.org/10.1371/journal.pgen.1008110
- National Clinical Guideline Centre (UK). (2013). Varicose Veins in the Legs: The Diagnosis and Management of Varicose Veins. London: National Institute for Health and Care Excellence (UK); (NICE Clinical Guidelines, No. 168.) 8, Conservative Management. Available from: https://www.ncbi.nlm.nih.gov/books/NBK328015/
- Yun, M. J., Kim, Y. K., Kang, D. M., Kim, J. E., Ha, W. C., Jung, K. Y., & Choi, H. W. (2018). A Study on Prevalence and Risk Factors for Varicose Veins in Nurses at a University Hospital. Safety and health at work, 9(1), 79–83. https://doi.org/10.1016/j.shaw.2017.08.005
- Chen, J.C. (2017). Current therapy for primary varicose veins. BCMJ, 59(8), 418-423.
- Lim, C. S., & Davies, A. H. (2014). Graduated compression stockings. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 186(10), E391–E398. https://doi.org/10.1503/cmaj.131281
- Motykie, G. D., Caprini, J. A., Arcelus, J. I., Reyna, J. J., Overom, E., & Mokhtee, D. (1999). Evaluation of therapeutic compression stockings in the treatment of chronic venous insufficiency. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.], 25(2), 116–120. https://doi.org/10.1046/j.1524-4725.1999.08095.x
- Health Quality Ontario (2019). Compression Stockings for the Prevention of Venous Leg Ulcer Recurrence: A Health Technology Assessment. Ontario health technology assessment series, 19(2), 1–86.
- Partsch, H., et al. (2008). Classification of Compression Bandages: Practical Aspects. Dermatologic surgery : official publication for American Society for Dermatologic Surgery, 34, 600-609. https://doi.org/10.1111/j.1524-4725.2007.34116.x
- Wade, R., Paton, F., Rice, S., Stansby, G., Millner, P., Flavell, H., Fox, D., & Woolacott, N. (2016). Thigh length versus knee length antiembolism stockings for the prevention of deep vein thrombosis in postoperative surgical patients; a systematic review and network meta-analysis. BMJ open, 6(2), e009456. https://doi.org/10.1136/bmjopen-2015-009456
- Rabe, E., Partsch, H., Hafner, J., Lattimer, C., Mosti, G., Neumann, M., Urbanek, T., Huebner, M., Gaillard, S., & Carpentier, P. (2018). Indications for medical compression stockings in venous and lymphatic disorders: An evidence-based consensus statement. Phlebology, 33(3), 163–184. https://doi.org/10.1177/0268355516689631
- Ziaja, D., Kocełak, P., Chudek, J., & Ziaja, K. (2011). Compliance with compression stockings in patients with chronic venous disorders. Phlebology, 26(8), 353–360. https://doi.org/10.1258/phleb.2010.010086



