Pictured below is a healthy vein (left side) and an unhealthy vein (right side). The unhealthy vein is suffering from venous insufficiency. Venous insufficiency is a medical term for vein disease. One of the symptoms of venous insufficiency is varicose veins.
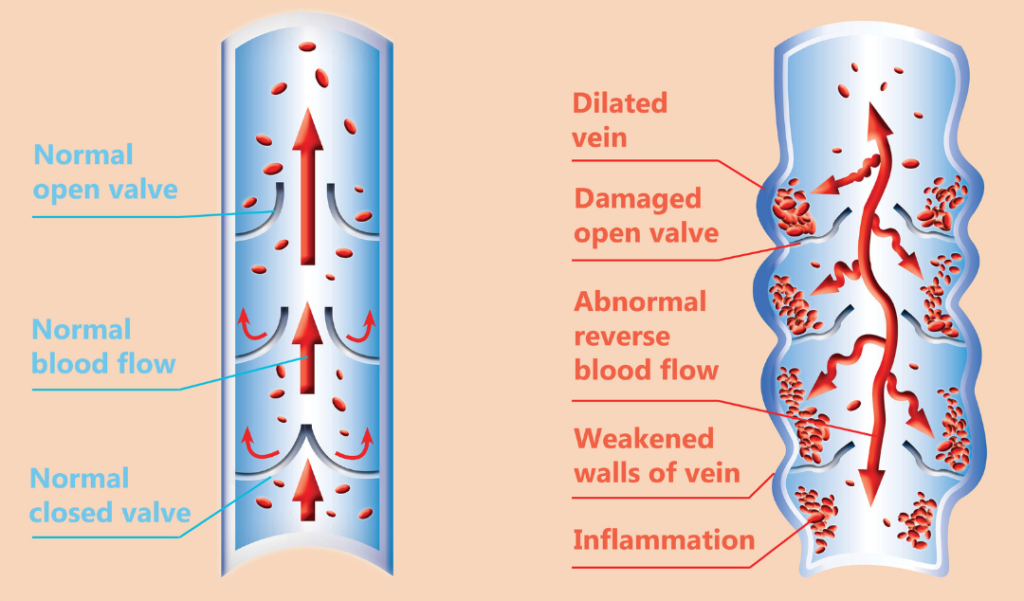
Varicose veins are bulging veins caused by poorly functioning valves or vein walls that have lost their elasticity. (1) With poor elasticity, veins can no longer effectively pump blood, causing reflux or pooling of the blood in the legs.
Approximately 20% of the global adult population will get varicose veins in their lifetime. (1) Women are more prone to varicose veins than men. About 22 million women and 11 million men between the ages of 40 and 80 are affected in the US alone. (2)
For some people, varicose veins are an unsightly nuisance. For others, they can cause leg cramping, aching, heavy or tired legs. The latter may be a sign of a more severe problem.
Below is a list of the hidden dangers varicose veins may cause if left untreated.
Table of Contents
ToggleHidden Dangers of Varicose Veins
Edema
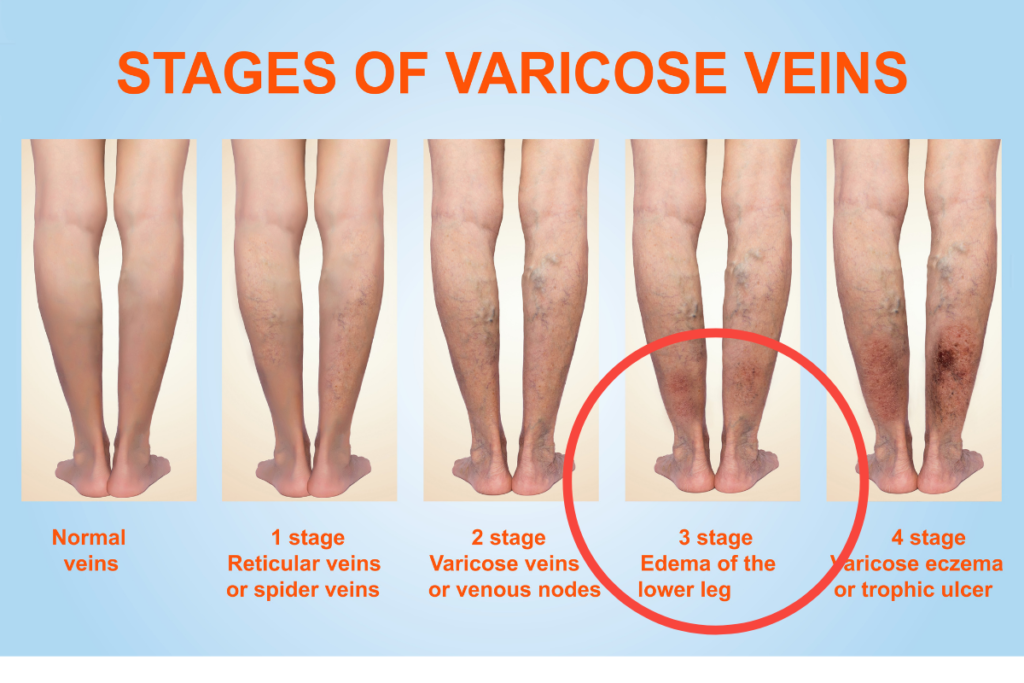
Edema is a medical term for leg swelling. Leg swelling may occur in patients with varicose veins due to the pressure that builds up within the veins. Fluid from the blood can leak into the surrounding tissue.
Your skin may even leak the fluid, which can appear clear or yellowish. As a result, this can lead to changes in skin color and hardening of the skin.
If the swelling is severe enough, you may find yourself not being able to put on shoes.
Varicose Eczema

Varicose eczema is a skin disorder that can occur in people who have varicose veins. Skin can become dry, cracked, shiny, and itchy. Further symptoms may develop such as purple or red sores, and venous ulcers on the lower legs.
When skin tissue is stretched from swelling, this can interfere with the body’s ability to defend itself from infection. Bacteria that are present on the surface of the skin are able to enter the body and can cause a skin infection called Cellulitis.
Cellulitis is a skin infection that can spread to other areas of the body. It can cause high fever or chills, nausea, vomiting, enlarging or hardening of the reddened area, increased pain, and numbness. In rare cases, individuals may require surgery to remove the dead skin tissue.
Hemorrhage

Since there is a more significant amount of blood pooling below the skin’s surface, trauma to the leg such as a cut or hit can cause a substantial amount of bleeding. Bleeding may sometimes occur spontaneously as well.
Patients with advanced age may be at a higher risk of spontaneous bleeding due to thin-walled veins. (3)
Individuals may first notice the problem when they feel blood running down their leg. As a result, they may also be feeling faint. It may take longer than usual for bleeding to stop if the injury is extensive, which can even be life-threatening.
Such was the case of a 66-year-old woman found dead in her home, surrounded by a large quantity of blood. The cause? Massive bleeding from ruptured varicosity. (4)
Thrombophlebitis

Thrombophlebitis is inflammation of a vein caused by a blood clot. Thrombophlebitis usually occurs in the superficial veins (veins closest to the skin). Symptoms may include swelling, unexplained limb pain or tenderness, redness of the skin, and difficulty walking.
Most bouts of superficial thrombophlebitis can last anywhere from two to six weeks. If the cause of superficial thrombophlebitis is associated with varicose veins, some individuals may have reoccurring episodes.
In some cases, thrombophlebitis may lead to deep vein thrombosis (DVT). This condition happens when the clot in the superficial vein extends further up to where the superficial veins and the deep veins meet.
Pulmonary Embolism

According to a recent study of 425,968 adults, varicose veins significantly increase the risk of deep vein thrombosis. (5)
Deep vein thrombosis (DVT) occurs when a blood clot forms in one or more of the deep veins in your body (typically in your legs). DVT may cause leg pain and swelling but can also occur with no symptoms.
If the blood clot in your deep veins breaks away, it can travel to your lungs. This condition is known as pulmonary embolism.
How does this happen, and why is it deadly? First, let’s understand how our body works.
Blood from your legs first travels up to your heart. The heart pumps the blood into your lungs through the pulmonary arteries.
The pulmonary arteries are blood vessels that carry blood from the right side of the heart through to the lungs’ capillaries. Your lungs then supply the blood with oxygen.
If a blood clot gets clogged in one of the arteries that go from the heart to the lungs, it can cause severe damage to your lungs and deprive oxygen levels in your blood.
The lack of oxygen can harm other organs in your body. If the blockage is significant, pulmonary embolism can lead to death.
Treatment

If you’re an individual who experiences pain when walking, sitting, or standing, these may be signs of venous insufficiency.
Luckily, venous insufficiency is a medical problem that is treatable by a safe, minimally invasive treatment, which has zero downtime and is covered by insurance.
The first step is getting an ultrasound by a vascular ultra-tech who is specifically trained to look for signs of venous reflux (the medical term for veins that no longer circulate blood properly).
If reflux is present, then a treatment called radiofrequency ablation can be performed by a vein specialist. This non-surgical treatment uses gentle heat to collapse the damaged vein. The collapsed vein gets reabsorbed by the body, and you get back to living pain-free.
Patients report minimal discomfort and get back to activities the very same day. Don’t wait any longer. Take action and avoid potentially harmful consequences down the road.
Elite Vein Clinic has successfully treated hundreds of happy individuals who no longer feel pain and discomfort in their legs.
To schedule an appointment with one of our health advisors, click the link below and fill out the information.
Someone from our clinic will reach out immediately and answer any questions you may have.
Book free consultation with a health advisor today.
—
References
- Antani, M.R., Dattilo, J.B. (2020) Varicose Veins. StatPearls. Treasure Island (FL): StatPearls Publishing https://www.ncbi.nlm.nih.gov/books/NBK470194/
- Piazza, G. (2014). Varicose veins. Retrieved from https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.113.008331#:~:text=Approximately%2023%25%20of%20US%20adults%20have%20varicose%20veins.&text=If%20spider%20telangiectasias%20and%20reticular,men%20and%2085%25%20of%20women.&text=Generally%20more%20common%20in%20women,of%2040%20to%2080%20years.
- Nicholls SC. Sequelae of untreated venous insufficiency. Seminars in interventional radiology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3036289/#r22162-6. Published September 2005.
- Fragkouli, Kleio, et al. “Unusual death due to a bleeding from a varicose vein: a case report.” BMC Research Notes, vol. 5, no. 1, 2012.https://bmcresnotes.biomedcentral.com/articles/10.1186/1756-0500-5-488.
- Shyue-Luen Chang, M. (2018, February 27). Varicose veins and Incident venous Thromboembolism (VTE) or PERIPHERAL artery Disease (PAD). Retrieved May 10, 2021, from https://jamanetwork.com/journals/jama/article-abstract/2673551

