Veins play a key role in your body. They ensure blood and nutrients flow throughout your body and back to your heart.
But sometimes genetics, age, or lifestyle factors impact vein health. Veins no longer work as well as they should. This can lead to a condition called varicose veins.
There is a good chance that someone you know lives with varicose veins. 22 million women and 11 million men between 40 and 80 have this condition(2).
Varicose veins can be a cosmetic annoyance for some, but they could also be a sign of bigger problems down the road. Let’s learn more about the causes, signs, and symptoms, as well as diagnosis and treatment options, for varicose veins.
Table of Contents
ToggleStructure of Veins
Before we get into varicose veins, we have to learn a little about veins themselves.
Your veins carry blood up toward the heart with help from your muscles, gravity, and by pumping your feet(1).
Vein walls consist of three layers – intima, media, and adventitia.
- The venous intima, the innermost layer, helps blood pass through your body smoothly(2).
- The venous media refers to the middle layer. This layer consists of elastic tissues and muscle(2), which allows the vein to change size without changing pressure(1).
- The adventitia layer is the outermost layer, made of collagen, elastic fibers, and fibroblasts(1). This gives the veins their shape and support(2).
Now that we understand the basics, let’s learn more about what causes issues in our veins.
What Causes Vein Disease?
Varicose veins are an example of venous insufficiency: when your body has trouble sending blood back to the heart(3).
Many factors can cause vein damage, but too much pressure is often the culprit(4).
Healthy veins pump blood up to your heart. But when veins struggle to do so, the pressure in these veins increases, leading to stretching, splitting, or thinning(5) of the vein structures.
The video above shows how increased pressure, also called venous hypertension, can result in this condition.
Sometimes the pressure comes from standing or sitting means the lower limbs are inactive, which can increase venous hypertension since your muscles are not pumping blood upward.
The mechanisms continue to impact each other, leading to blue or purple veins that protrude from beneath the skin: varicose veins.
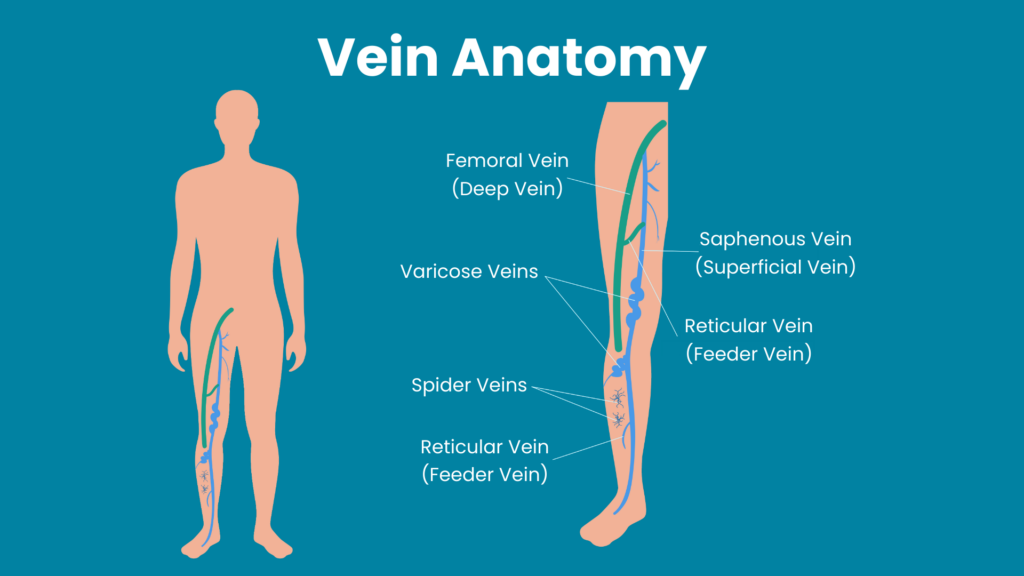
Varicose veins occur mostly in the lower extremities because these veins are located furthest from the heart. They are often superficial, deep, or perforating veins(1).
Risk Factors for Varicose Veins

Who is most likely to develop this condition? There are a few risk factors to consider.
Hormones and Pregnancy
Large amounts of estrogen can cause veins to swell, putting you at risk for varicose veins.
Pregnancy hormones can also impact vein health. Progesterone causes venous dilation, which can weaken veins(10). Weight gain also adds additional pressure(11).
Lifestyle
If your job has you on your feet or sitting at a desk all day, you may be more at risk for developing this condition. Smoking can also increase your risk: it damages the walls of veins and can cause inflammation(8).
Obesity
Obesity puts more weight on the lower limbs, which can lead to venous hypertension(2).
Deep Vein Thrombosis
A history of deep vein thrombosis is also a risk factor for developing varicose veins. Deep vein thrombosis, or DVT, occurs when a blood clot forms deep in the veins(2).
Age
As we age, our bodies experience wear and tear, including our veins. The valves become less efficient, leading to the possibility of varicose veins(2).
Genetics
If a family member has varicose veins, you might develop them too. Certain genes impact vein function, making veins more susceptible to damage(12). Other diseases in the family increase your risk of developing varicose veins. Examples include Ehlers-Danlos syndrome or Klippel-Trenaunay syndrome(12).
Signs and Symptoms of Varicose Veins
Varicose veins look blue or purple and may bulge from under the skin. They are sometimes described as “spider veins.”
In addition to their appearance, you may feel heaviness, burning, or throbbing in your legs, or notice skin changes in the area. You might notice pain after prolonged sitting or standing as well.
In some cases, you may also have venous ulcers, or experience Restless Legs Syndrome.
If you experience any of the above signs or symptoms, talk to your doctor. You may have varicose veins.
Getting a Diagnosis
If you suspect you have varicose veins, it’s time to talk to your doctor. They will evaluate your medical history and perform a physical exam.
Imaging is essential when diagnosing this condition. There are two methods they may use:
Venous duplex ultrasound scan: This is a safe, non-invasive diagnostic scan that uses sound waves to measure the speed of blood flow in the lower limbs(13).
Doppler ultrasonography: A high-frequency sound wave helps measure blood flow through vessels throughout your whole body(15).
With these exams, the doctor can evaluate your vein health and reach a diagnosis(14).
Are Varicose Veins Dangerous?
Varicose veins themselves can be fine on their own but can be a sign of dangers to come. If you are diagnosed, your doctor will tell you to monitor your symptoms. Varicose veins can be a sign of chronic venous insufficiency, meaning your veins are not working as well as they should.
Chronic venous insufficiency can lead to venous ulcerations, which can be dangerous – and, when left untreated, can lead to more complications.
In addition to possible bleeding(16), this can lead to superficial thrombophlebitis(18), complicating blood clot formation. This is painful, but not necessarily life-threatening.
However, superficial thrombophlebitis can develop into a deep vein clot known as deep vein thrombosis, or DVT. DVT is dangerous and requires immediate medical attention. This could progress to a pulmonary embolism, which can be fatal.
Preventing Varicose Veins
There is no way to fully prevent varicose veins, but there are measures you can take to reduce your chances of developing them in the first place:
Exercise
Exercise improves blood flow in your legs as leg muscles pump. Your calves squeeze your veins, pushing blood to the heart. Flexing these muscles helps keep veins healthy.
Weight management
If you are overweight, losing weight can lessen the burden on the lower extremities and reduce venous hypertension.
Eating a vein-healthy diet
Eating a high-fiber, low-salt diet is good for your veins! Too much salt can lead to higher blood pressure, increasing the risk of having hypertension and cardiovascular diseases(19).
Elevate your legs
Lifting your legs up decreases the pressure that gravity causes and helps blood flow back to the heart.
Frequently changing your sitting or standing position
Avoid too much sitting or standing. Changing your position triggers the pumping action of the muscles on your legs.
Treating Varicose Veins

There are several treatment options available for varicose veins:
Compression Therapy
Compression therapy is essential for treating varicose veins. This is often the first step patients take. Pressure is applied to the leg to reduce venous insufficiency(4).
Radiofrequency Ablаtіоn
Radiofrequency Ablаtіоn (RFA) is a minimally invasive procedure performed inside the vein. This outpatient procedure uses thermal energy to treat the vein. This treatment has fewer complications than most(17) and is often recommended for larger varicose veins.
Sclerotherapy
Sclerotherapy is a procedure for small and mid-sized varicose veins. It involves inserting a solution into the veins(17). This sclerosing solution closes up the veins. Patients should wear compression stockings after this procedure.
Endovenous Thermoablation
Endovenous thermoablation is another minimally invasive option. The doctor inserts a catheter to deliver thermal energy to close off the vein(17). This is an outpatient and cost-effective treatment option.
Ambulatory Phlebectomy
This procedure involves a series of small skin punctures. Localized anesthesia is given beforehand. This is recommended for patients with side branch varicose veins, and varicose veins near the foot, ankle, or knee pit(17).
Conclusion
Varicose veins may simply be a cosmetic concern. However, this condition could also signify bigger medical issues one day. It’s important to know the signs and symptoms of this condition. If it affects you or a loved one now or in the future, you’ll be equipped with the knowledge to seek a diagnosis and get the best treatment possible.
Elite Vein Clinic is your go-to Valley vein health specialist. Our experts use the latest medical technology and apply treatment with a patient-first approach. We offer minimally invasive vein treatments in Phoenix, Chandler, Gilbert, Mesa, Scottsdale, Tempe, and Peoria. Ready to treat your varicose veins? Book a free consultation today and take the first step toward a healthier you!
Book a consult today!
—
References
- Brunicardi F., Andersen D.K., Billiar T.R., Dunn D.L., Kao L.S., Hunter J.G., Matthews J.B., & Pollock R.E.(Eds.), (2019). Schwartz’s Principles of Surgery, 11e. McGraw-Hill. https://accesssurgery.mhmedical.com/content.aspx?bookid=2576§ionid=208294867
- Piazza, G. (2014). Varicose veins. Circulation: Clinical Summaries. 130(7), 582–587. https://doi.org/10.1161/CIRCULATIONAHA.113.008331
- Tucker, W.D., Arora Y., & Mahajan, K. (2020) Anatomy, Blood Vessels. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470401/
- Youn, Y. J., & Lee, J. (2019). Chronic venous insufficiency and varicose veins of the lower extremities. The Korean journal of internal medicine, 34(2), 269–283. https://doi.org/10.3904/kjim.2018.230
- Bergan JJ, Schmid-Schönbein GW, Smith PD, Nicolaides AN, Boisseau MR, Eklof B. Chronic venous disease.N Engl J Med. 2006; 355:488–498.
- Recek C. (2013). Calf pump activity influencing venous hemodynamics in the lower extremity. The International journal of angiology : official publication of the International College of Angiology, Inc, 22(1), 23–30. https://doi.org/10.1055/s-0033-1334092
- Ciardullo, A.V., et al. (2000). High endogenous estradiol is associated with increased venous distensibility and clinical evidence of varicose veins in menopausal women. Journal of vascular surgery. 32(3), 544-549. https://doi.org/10.1067/mva.2000.107768
- Gourgou, S., Dedieu, F., & Sancho-Garnier, H. (2002) Lower Limb Venous Insufficiency and Tobacco Smoking: A Case-Control Study. American Journal of Epidemiology. 155(11), 1007–1015. https://doi.org/10.1093/aje/155.11.1007
- Labropoulos, N. (2019). How Does Chronic Venous Disease Progress from the First Symptoms to the Advanced Stages? A Review. Adv Ther 36, 13–19. https://doi.org/10.1007/s12325-019-0885-3
- Mashiah, A., Berman, V., Thole, H. H., Rose, S. S., Pasik, S., Schwarz, H., & Ben-Hur, H. (1999). Estrogen and progesterone receptors in normal and varicose saphenous veins. Cardiovascular surgery (London, England), 7(3), 327–331. https://doi.org/10.1016/s0967-2109(98)00132-x
- Kominiarek, M. A., & Peaceman, A. M. (2017). Gestational weight gain. American journal of obstetrics and gynecology, 217(6), 642–651. https://doi.org/10.1016/j.ajog.2017.05.040
- Anwar, M.A., Georgiadis, K.A., Shalhoun, J., Lim, C.S., Gohel, M., & Davies, A.H. (2012). A review of familial, genetic, and congenital aspects of primary varicose vein disease. Circulation: Cardiovascular Genetics. 5(4), 460-466. https://doi.org/10.1161/CIRCGENETICS.112.963439
- Cheung M.E., & Firstenberg M.S. (2020) Duplex Ultrasound. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459266/
- Hwang J. Y. (2017). Doppler ultrasonography of the lower extremity arteries: anatomy and scanning guidelines. Ultrasonography (Seoul, Korea), 36(2), 111–119. https://doi.org/10.14366/usg.16054
- Moorthy R. S. (2002). Doppler ultrasound. Medical journal, Armed Forces India, 58(1), 1–2. https://doi.org/10.1016/S0377-1237(02)80001-6
- Tisi P. V. (2011). Varicose veins. BMJ clinical evidence, 2011, 0212.
- Campbell B. (2006). Varicose veins and their management. BMJ (Clinical research ed.), 333(7562), 287–292. https://=doi.org/10.1136/bmj.333.7562.287
- Czysz A., & Higbee S.L.(2020) Superficial Thrombophlebitis. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK556017/
- Aaron, K. J., & Sanders, P. W. (2013). Role of dietary salt and potassium intake in cardiovascular health and disease: a review of the evidence. Mayo Clinic proceedings, 88(9), 987–995. https://doi.org/10.1016/j.mayocp.2013.06.005



